Skin Cancer
Risk Factors for Merkel Cell Carcinoma Merkel cell carcinoma is one of the most aggressive forms of skin cancer due to its rapid growth and potential for metastasis. Knowing the factors that could increase its occurrence is a key step in defending your skin’s health. What Are the Risk Factors for Merkel Cell Carcinoma? These…
Read MoreDangers of Merkel Cell Carcinoma Merkel cell carcinoma is a very rare type of skin cancer—but it’s also one of the most aggressive. What is Merkel Cell Carcinoma Skin Cancer? Merkel cell carcinoma (MCC) is named after the Merkel cells, which are located at the base of the outermost layer of the skin. Merkel cells…
Read MoreTreatments for Skin Cancer Surgical interventions have long dominated the treatment of skin cancer. However, there are also several non-surgical treatments for skin cancer that have developed as the medical world has learned more about this complex condition. Topical Treatments for Skin Cancer Also known as chemotherapy cream, topical treatments for skin cancer are applied…
Read MoreSurgery for Skin Cancer Skin cancer has layers of complexity that can affect a dermatologist’s approach in terms of diagnosis and treatment. One of the most commonly asked questions about skin cancer treatment is whether or not a patient will require surgery. Although the answer ultimately requires a doctor’s consultation, here are some general guidelines…
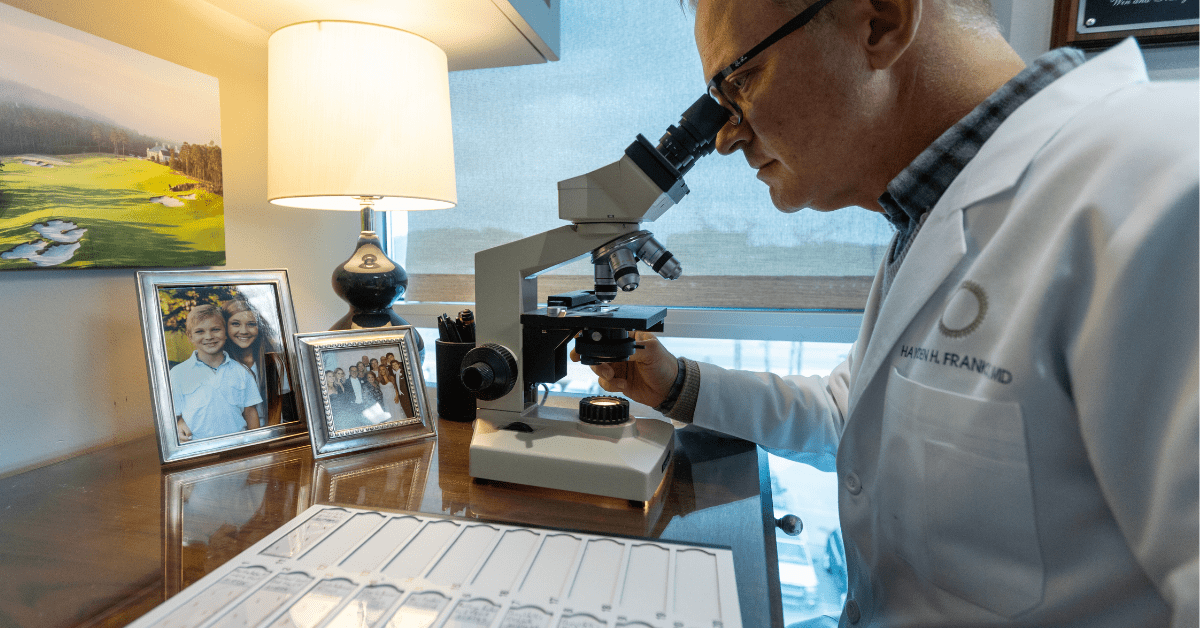
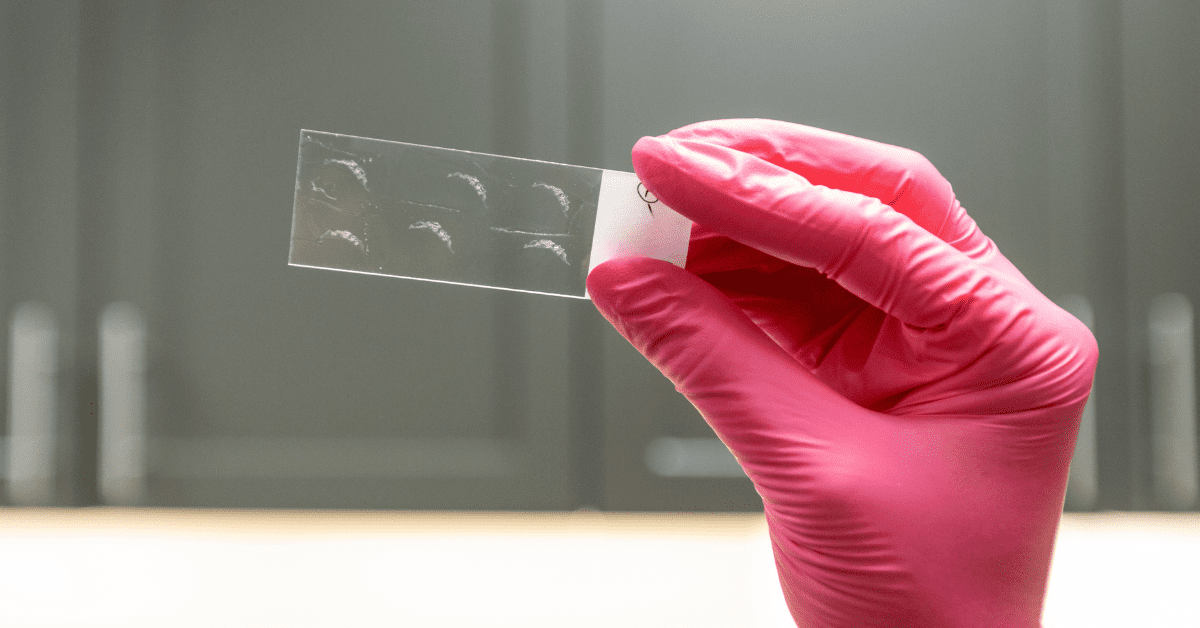
Read MoreSkin Cancer Biopsy Picture this: you notice a suspicious spot on your skin—a freckle that has changed in shape, a mole that looks irregular, or a lesion that doesn’t seem to heal. You schedule an appointment with a healthcare professional. After a thorough examination, they suggest a skin cancer biopsy. But what exactly does that…
Read MoreSkin Biopsy Procedures Skin cancer affects millions of people globally, as well as countless loved ones and partners who accompany them on their journey. Because of the potentially significant consequences, it is critical that they be addressed swiftly and correctly. To achieve that result, precise skin cancer detection and therapy rely primarily on skin biopsy…
Read MoreSkin Cancer Prevention Skin cancer prevention can feel onerous. So, which prevention tips make the biggest difference? Skin cancer is an extremely common form of cancer, affecting millions of people worldwide each year. In fact, 1 in 5 Americans will contract some form of skin cancer before the age of 70. The good news is…
Read MoreSquamous Cell Carcinoma Squamous cell carcinoma skin cancer can be mistaken for other common skin conditions. Understanding Squamous Cell Carcinoma Squamous cell carcinoma (SCC) forms a malignant tumor arising from epidermal keratinocytes. Most of the time, SCC comes from sun damage. SCC is more aggressive than basal cell carcinoma and has a higher potential to…
Read MoreBasal Cell Carcinoma The most common form of skin cancer, basal cell carcinoma is often caused by prolonged exposure to UV radiation from the sun or tanning beds. It can also occur in areas of your skin previously compromised by radiation therapy, burns, or inflammation. Understanding Basal Cell Carcinoma Basal cell carcinoma (BCC) develops in…
Read MoreMelanoma Melanoma is considered the most severe type of skin cancer. It’s important to recognize the signs of melanoma so you can alert your doctor about any suspicious areas on your skin. Understanding Melanoma Melanoma occurs when the cells responsible for producing the pigment of our skin turn cancerous. Although it affects people of any age,…
Read More